Transforming Cancer Care with Transplant Oncology
Robotic Surgery for Enhanced Precision, Faster Recovery, and Improved Patient Outcomes.
Miami Transplant Institute offers new hope for patients with cancer through a joint collaboration between Jackson Health System and Sylvester Comprehensive Cancer Center, part of UHealth – University of Miami Health System. Through liver transplantation, transplant oncology aims at partially or completely replacing cancer cells with healthy tissue from a donor, allowing patients to regain liver function or be cured of their cancer. Those with cholangiocarcinoma, hepatocellular carcinoma, neuroendocrine tumors, or non-resectable metastatic colon cancer to the liver can now be treated outside of the previous criteria, and be considered for a liver transplant.

Hepatocellular Carcinoma
Cholangiocarcinoma
Metastatic Colon Cancer to the Liver
Neuroendocrine Tumors
Support Groups
Miami Transplant Institute offers new hope for patients with cancer through a joint collaboration between Jackson Health System and Sylvester Comprehensive Cancer Center, part of UHealth – University of Miami Health System. Through liver transplantation, transplant oncology aims at partially or completely replacing cancer cells with healthy tissue from a donor, allowing patients to regain liver function or be cured of their cancer. Those with cholangiocarcinoma, hepatocellular carcinoma, neuroendocrine tumors, or non-resectable metastatic colon cancer to the liver can now be treated outside of the previous criteria, and be considered for a liver transplant.
Hepatocellular Carcinoma
Cholangiocarcinoma
Metastatic Colon Cancer to the Liver
Neuroendocrine Tumors
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is a type of liver cancer that originates in hepatocytes, the functional cells of the liver. Symptoms of HCC include abdominal pain or swelling, unintentional weight loss, loss of appetite, vomiting and nausea, fatigue, and jaundice, which is the yellowing of the skin and eyes. However, sometimes HCC may not show symptoms until it reaches a more advanced stage. It is a challenging cancer to treat and one of the leading causes of cancer-related deaths globally.
Regardless of its etiology, cirrhosis is the most significant risk factor for HCC. In the United States, alcohol consumption is the most critical risk factor for cirrhosis and HCC. Chronic hepatitis B and C infections, obesity, and diabetes are also significant risk factors.
Diagnosis of HCC typically involves a combination of medical history assessments, radiological exams such as ultrasound, CT, and MRI scans, and laboratory examinations. In some cases, a liver biopsy may be necessary to confirm the diagnosis.
While multiple therapeutic modalities exist, such as chemotherapy, radiotherapy, and targeted therapies, only surgical resection and transplantation offer a curative perspective. In many cases, resection is not an option due to the diffuse involvement of the liver, making it impossible to isolate a functional, healthy area. In such cases, liver transplantation is often the best option. During this surgery, the patient’s neoplastic liver is removed and replaced with a healthy liver. If the disease is confined to the liver alone, this cancer can be cured.
The criteria for determining a patient’s eligibility for liver transplantation depend on several factors, such as the patient’s overall health, characteristics and number of tumors, the existence of disease outside the liver, donor availability, and others. That is why early patient evaluation is crucial, as the same patient can become non-transplantable quickly.
In the past, the Milan Criteria were used to determine a patient’s eligibility for transplantation. These criteria dictated that only patients with a tumor size of 5 cm or smaller, or three tumors smaller than or equal to 3 cm, were eligible. Patients meeting the Milan Criteria have a five-year survival rate of almost 91%.
However, advances in research have expanded the criteria to include more severe cases with excellent results. Miami Transplant Institute’s criteria allow patients beyond the Milan criteria to be treated and possibly cured. Through an individual assessment of each patient by our specialized oncology transplant team, the indication for this treatment and surgical planning can be evaluated.
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is a type of liver cancer that originates in hepatocytes, the functional cells of the liver. Symptoms of HCC include abdominal pain or swelling, unintentional weight loss, loss of appetite, vomiting and nausea, fatigue, and jaundice, which is the yellowing of the skin and eyes. However, sometimes HCC may not show symptoms until it reaches a more advanced stage. It is a challenging cancer to treat and one of the leading causes of cancer-related deaths globally.
Regardless of its etiology, cirrhosis is the most significant risk factor for HCC. In the United States, alcohol consumption is the most critical risk factor for cirrhosis and HCC. Chronic hepatitis B and C infections, obesity, and diabetes are also significant risk factors.
Diagnosis of HCC typically involves a combination of medical history assessments, radiological exams such as ultrasound, CT, and MRI scans, and laboratory examinations. In some cases, a liver biopsy may be necessary to confirm the diagnosis.
While multiple therapeutic modalities exist, such as chemotherapy, radiotherapy, and targeted therapies, only surgical resection and transplantation offer a curative perspective. In many cases, resection is not an option due to the diffuse involvement of the liver, making it impossible to isolate a functional, healthy area. In such cases, liver transplantation is often the best option. During this surgery, the patient’s neoplastic liver is removed and replaced with a healthy liver. If the disease is confined to the liver alone, this cancer can be cured.
The criteria for determining a patient’s eligibility for liver transplantation depend on several factors, such as the patient’s overall health, characteristics and number of tumors, the existence of disease outside the liver, donor availability, and others. That is why early patient evaluation is crucial, as the same patient can become non-transplantable quickly.
In the past, the Milan Criteria were used to determine a patient’s eligibility for transplantation. These criteria dictated that only patients with a tumor size of 5 cm or smaller, or three tumors smaller than or equal to 3 cm, were eligible. Patients meeting the Milan Criteria have a five-year survival rate of almost 91%.
However, advances in research have expanded the criteria to include more severe cases with excellent results. Miami Transplant Institute’s criteria allow patients beyond the Milan criteria to be treated and possibly cured. Through an individual assessment of each patient by our specialized oncology transplant team, the indication for this treatment and surgical planning can be evaluated.
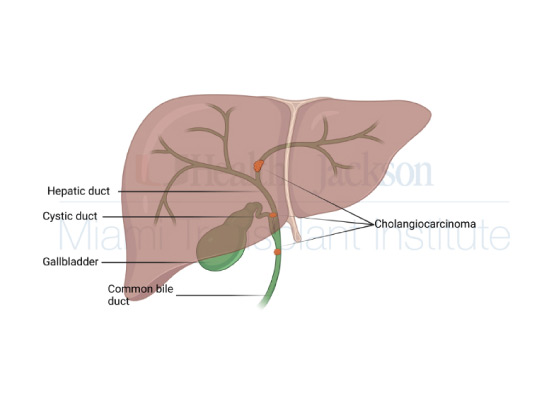
Cholangiocarcinoma
Cholangiocarcinoma is a neoplasm that affects specific portions of the bile duct, the tubes that carry bile from the liver to the small intestine to help with the digestion of food. It is usually classified based on the anatomical subtype, that is, on the location of the neoplasm, into intrahepatic (when the affected ducts are those located inside the liver), perihilar (in the region of the hepatic Hilum) and distal (farther from the liver). Despite its increasing incidence in recent decades worldwide, it is considered a rare neoplasm.
It is common for cholangiocarcinoma not to show clear symptoms until it reaches a more advanced stage. Still, the most common symptoms are Unexplained weight loss, abdominal pain, jaundice (yellowing of the eyes and skin), nausea, vomiting, and itching. The most common risk factors depend on the place in the world, but in the US, they are choledocholithiasis, cholelithiasis, primary sclerosing cholangitis, biliary cirrhosis, inflammatory bowel disease, and primary sclerosing cholangitis.
The diagnosis is made through clinical history, imaging tests, such as CT scans, MRIs, endoscopies, and sometimes biopsies, usually collected via endoscopic examination of the bile duct. Even the diagnosis depends on the anatomical subtype since each type has symptoms and allows different tests.
The treatment of cholangiocarcinoma can be diverse. Usually, radiotherapies and chemotherapies aim at reducing the tumor and relieving symptoms. But surgery is the main modality of treatment. Through resection or, in more diffuse cases, transplantation, patients can have a curative perspective. The indication varies according to the patient and the tumor’s characteristics, so a case-by-case evaluation with a specialist transplant oncology team is necessary.
The Transplant Oncology team at the Miami Transplant Institute developed its own criteria for Cholangiocarcinoma patients, providing state-of-the-art medicine to patients that priorly had no options.
Cholangiocarcinoma
Cholangiocarcinoma is a neoplasm that affects specific portions of the bile duct, the tubes that carry bile from the liver to the small intestine to help with the digestion of food. It is usually classified based on the anatomical subtype, that is, on the location of the neoplasm, into intrahepatic (when the affected ducts are those located inside the liver), perihilar (in the region of the hepatic Hilum) and distal (farther from the liver). Despite its increasing incidence in recent decades worldwide, it is considered a rare neoplasm.
It is common for cholangiocarcinoma not to show clear symptoms until it reaches a more advanced stage. Still, the most common symptoms are Unexplained weight loss, abdominal pain, jaundice (yellowing of the eyes and skin), nausea, vomiting, and itching. The most common risk factors depend on the place in the world, but in the US, they are choledocholithiasis, cholelithiasis, primary sclerosing cholangitis, biliary cirrhosis, inflammatory bowel disease, and primary sclerosing cholangitis.
The diagnosis is made through clinical history, imaging tests, such as CT scans, MRIs, endoscopies, and sometimes biopsies, usually collected via endoscopic examination of the bile duct. Even the diagnosis depends on the anatomical subtype since each type has symptoms and allows different tests.
The treatment of cholangiocarcinoma can be diverse. Usually, radiotherapies and chemotherapies aim at reducing the tumor and relieving symptoms. But surgery is the main modality of treatment. Through resection or, in more diffuse cases, transplantation, patients can have a curative perspective. The indication varies according to the patient and the tumor’s characteristics, so a case-by-case evaluation with a specialist transplant oncology team is necessary.
The Transplant Oncology team at the Miami Transplant Institute developed its own criteria for Cholangiocarcinoma patients, providing state-of-the-art medicine to patients that priorly had no options.
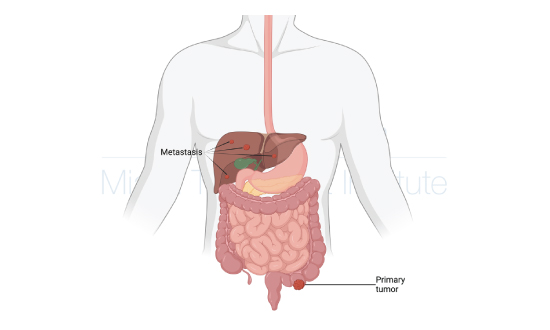
Colorectal Carcinoma
Colorectal cancer is a type of cancer that affects the colon or rectum, which are parts of the large intestine. It is the third most commonly diagnosed cancer in men and women and the second leading cause of cancer deaths in the United States.
Colorectal cancer can develop from small growths called polyps, which can be discovered during routine screening exams. These polyps can become cancerous over time, so early detection and removal of them is crucial. Some common symptoms of colorectal cancer include changes in bowel habits, rectal bleeding, abdominal pain, and unintended weight loss.
Certain risk factors can increase the likelihood of developing colorectal cancer, such as age, family history of colorectal cancer, personal history of inflammatory bowel disease, and certain genetic mutations. Adopting a healthy lifestyle, such as maintaining a healthy weight, engaging in regular physical activity, and eating a balanced diet with plenty of fruits, vegetables, and whole grains, may help reduce the risk of developing colorectal cancer.
Screening for colorectal cancer is recommended for average-risk individuals starting at age 45 or 50, depending on the guidelines. Screening tests may include a stool-based test, flexible sigmoidoscopy, colonoscopy, or other imaging tests. The type and frequency of screening tests may vary depending on an individual’s risk factors and personal health history.
50% of all the patients with colorectal cancer developed metastasis to the liver at some point in their diseases. Because the symptoms can be very non-specific, 25% of the patients at the diagnosis already have metastasis. These metastases can generate various symptoms and decrease the patient’s hepatic function and survival.
A transplant is an important option to be considered for patients with colorectal cancer with metastasis to the liver. Through transplant oncology, a specialized team can evaluate the patient and tumor’s characteristics to assess the feasibility and gains of a possible transplant, changing the neoplastic liver to
Colorectal Carcinoma
Colorectal cancer is a type of cancer that affects the colon or rectum, which are parts of the large intestine. It is the third most commonly diagnosed cancer in men and women and the second leading cause of cancer deaths in the United States.
Colorectal cancer can develop from small growths called polyps, which can be discovered during routine screening exams. These polyps can become cancerous over time, so early detection and removal of them is crucial. Some common symptoms of colorectal cancer include changes in bowel habits, rectal bleeding, abdominal pain, and unintended weight loss.
Certain risk factors can increase the likelihood of developing colorectal cancer, such as age, family history of colorectal cancer, personal history of inflammatory bowel disease, and certain genetic mutations. Adopting a healthy lifestyle, such as maintaining a healthy weight, engaging in regular physical activity, and eating a balanced diet with plenty of fruits, vegetables, and whole grains, may help reduce the risk of developing colorectal cancer.
Screening for colorectal cancer is recommended for average-risk individuals starting at age 45 or 50, depending on the guidelines. Screening tests may include a stool-based test, flexible sigmoidoscopy, colonoscopy, or other imaging tests. The type and frequency of screening tests may vary depending on an individual’s risk factors and personal health history.
50% of all the patients with colorectal cancer developed metastasis to the liver at some point in their diseases. Because the symptoms can be very non-specific, 25% of the patients at the diagnosis already have metastasis. These metastases can generate various symptoms and decrease the patient’s hepatic function and survival.
A transplant is an important option to be considered for patients with colorectal cancer with metastasis to the liver. Through transplant oncology, a specialized team can evaluate the patient and tumor’s characteristics to assess the feasibility and gains of a possible transplant, changing the neoplastic liver to
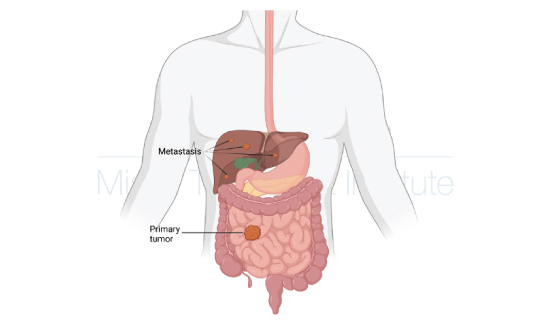
Neuroendocrine Tumors
Neuroendocrine tumors arise from neuroendocrine cells found throughout the body, with a high concentration in the gastrointestinal tract and lungs. Although they are relatively rare, the incidence of these tumors has been on the rise for the past few decades. When the cancer originates from the gastroenteropancreatic (GEP) region, it is classified as a GEP-NET.
Symptoms of neuroendocrine tumors can vary significantly depending on the tumor’s primary site and specific characteristics. Some common symptoms include abdominal pain, diarrhea, flushing, wheezing, and weight loss. However, some patients may not experience symptoms until the tumor has grown or spread to other body parts.
Neuroendocrine tumors are a complex type of cancer to treat, and multiple therapeutic modalities are available. The treatment approach will depend on the tumor’s characteristics and the patient’s overall health. Surgery is often the primary treatment for neuroendocrine tumors. However, if the tumor has spread or cannot be surgically removed, other treatment options may be used, such as chemotherapy, radiation therapy, and targeted therapy.
For some patients, liver transplantation may be the best treatment option. This is especially true for those with advanced liver neuroendocrine tumors or multiple liver metastases. A liver transplant can replace the neoplastic liver with a healthy one, potentially curing the disease. The Miami Transplant Institute has developed specific criteria to evaluate neuroendocrine tumor patients who may benefit from transplantation.
Neuroendocrine tumors can be challenging to diagnose and treat. But, with the help of specialized oncology teams, including Transplant Oncology specialists, patients can receive personalized care and access various treatment options, including liver transplantation, which can offer a curative perspective.
Neuroendocrine Tumors
Neuroendocrine tumors arise from neuroendocrine cells found throughout the body, with a high concentration in the gastrointestinal tract and lungs. Although they are relatively rare, the incidence of these tumors has been on the rise for the past few decades. When the cancer originates from the gastroenteropancreatic (GEP) region, it is classified as a GEP-NET.
Symptoms of neuroendocrine tumors can vary significantly depending on the tumor’s primary site and specific characteristics. Some common symptoms include abdominal pain, diarrhea, flushing, wheezing, and weight loss. However, some patients may not experience symptoms until the tumor has grown or spread to other body parts.
Neuroendocrine tumors are a complex type of cancer to treat, and multiple therapeutic modalities are available. The treatment approach will depend on the tumor’s characteristics and the patient’s overall health. Surgery is often the primary treatment for neuroendocrine tumors. However, if the tumor has spread or cannot be surgically removed, other treatment options may be used, such as chemotherapy, radiation therapy, and targeted therapy.
For some patients, liver transplantation may be the best treatment option. This is especially true for those with advanced liver neuroendocrine tumors or multiple liver metastases. A liver transplant can replace the neoplastic liver with a healthy one, potentially curing the disease. The Miami Transplant Institute has developed specific criteria to evaluate neuroendocrine tumor patients who may benefit from transplantation.
Neuroendocrine tumors can be challenging to diagnose and treat. But, with the help of specialized oncology teams, including Transplant Oncology specialists, patients can receive personalized care and access various treatment options, including liver transplantation, which can offer a curative perspective.